Dental implants have revolutionized the way we approach the restoration of missing teeth, offering solutions that are not only functional but also aesthetically pleasing. Among the various types of dental implants available, endosteal implants stand out as the most commonly used and widely recognized standard in implant dentistry. Composed of materials like titanium and zirconia, these implants are surgically placed directly into the jawbone, serving as a sturdy foundation for replacement teeth. This blog aims to delve into the reasons behind the popularity and reliability of endosteal implants, exploring their advantages, the procedure involved in their placement, suitability criteria for patients, and how they compare with other dental implant options. By understanding why endosteal implants have become the gold standard in dental restorations, patients can make informed decisions about their dental care, ultimately leading to improved oral health and quality of life.
In This Blog:
- Understanding Endosteal Implants
- The Advantages of Endosteal Implants
- The Procedure of Placing Endosteal Implants
- Comparing Endosteal Implants with Other Restoration Types
- FAQs About Endosteal Implants
Understanding Endosteal Implants
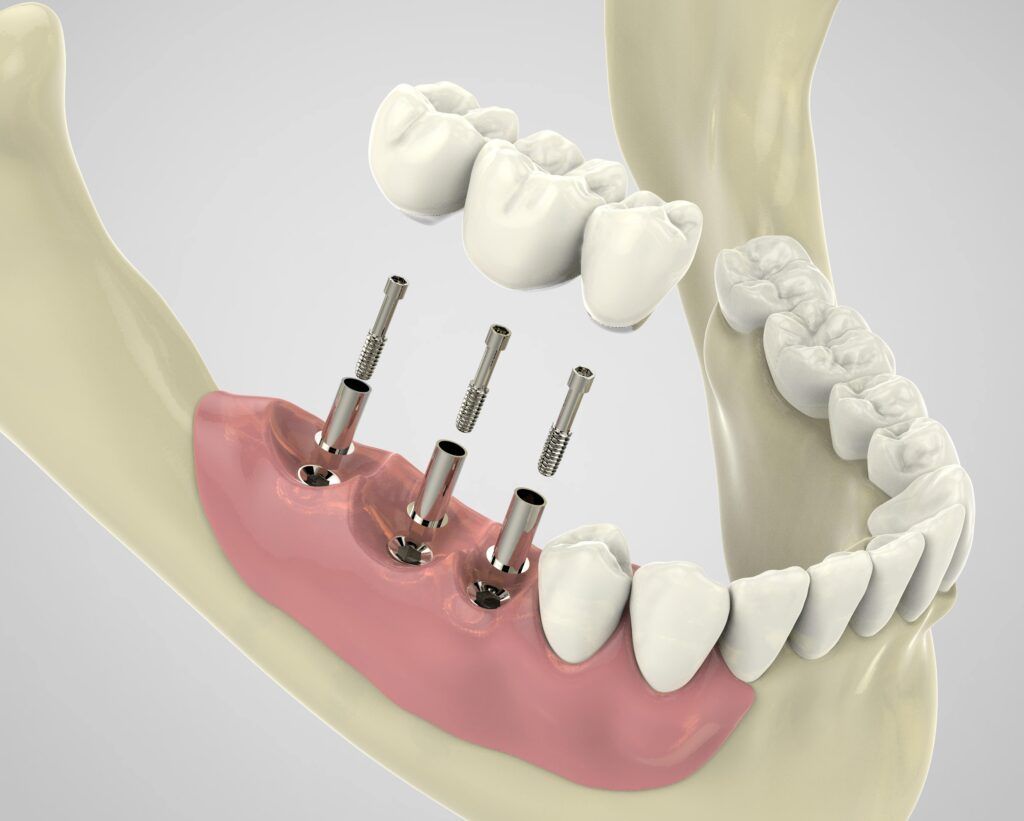
Endosteal implants are the cornerstone of modern implant dentistry, setting the standard for durability, functionality, and aesthetic integration. These implants are surgically placed directly into the jawbone, acting as an artificial root upon which replacement teeth or bridges can be mounted. The term “endosteal” refers to their placement inside the bone, distinguishing them from other types of dental implants that may sit on top of or alongside the jawbone.
The primary materials used in the construction of endosteal implants are titanium and zirconia. Titanium is celebrated for its strength, biocompatibility, and the unique ability to fuse with bone through a process known as osseointegration. This process allows the implant to become a permanent part of the jawbone, providing a stable and durable foundation for prosthetic teeth. Zirconia, while newer to the field, offers similar benefits with the added advantage of being metal-free, making it an attractive option for patients with metal sensitivities or those seeking a more natural-looking implant.
Osseointegration is central to the success of endosteal implants. Following the surgical placement of the implant into the jawbone, a period of healing allows the bone to grow around and bond with the implant, effectively locking it in place. This process not only ensures the stability of the implant but also helps preserve the jawbone and maintain the facial structure, preventing the bone loss that often accompanies tooth loss.
Endosteal implants can vary in shape and size, tailored to meet the specific needs of the patient and the anatomical considerations of their jawbone. The most common forms are screw-type implants, which resemble a screw, and cylinder-type implants, which are shaped like small cylinders. The choice between these types depends on the patient’s bone density, the location of the missing tooth, and other individual factors that a dental professional will evaluate during the planning stage of implantation.
Understanding the nature and benefits of endosteal implants is the first step for patients considering this reliable and long-lasting solution to tooth loss. By choosing endosteal implants, patients are investing in a future of confident smiles and improved oral health, underpinned by the most advanced technology in implant dentistry.
The Advantages of Endosteal Implants
Endosteal implants are widely recognized for their numerous benefits, making them a preferred choice for dental restoration. Their advantages extend beyond just replacing missing teeth; they contribute significantly to long-term oral health, functionality, and aesthetic appeal. Here are some of the key benefits that set endosteal implants apart:
Longevity and Durability:
One of the most compelling advantages of endosteal implants is their remarkable durability. Made from materials like titanium and zirconia, these implants are designed to last a lifetime with proper care and maintenance. Unlike dental bridges or dentures, which may need to be replaced every 5 to 10 years, endosteal implants offer a permanent solution to tooth loss.
Preservation of Jawbone and Facial Structure:
Tooth loss often leads to jawbone deterioration, which can cause the facial structure to sag over time. Endosteal implants stimulate the bone in the same way natural tooth roots do, promoting bone growth and preventing bone loss. This process, known as osseointegration, not only secures the implant in place but also helps maintain the integrity of the facial structure.
Improved Oral Health:
Unlike bridges, which require altering adjacent teeth, endosteal implants are placed directly into the jawbone, leaving surrounding teeth untouched. This feature minimizes potential damage to neighboring teeth and supports overall oral health. Additionally, implants make it easier to maintain good oral hygiene, as they can be brushed and flossed just like natural teeth.
Enhanced Comfort and Functionality:
Endosteal implants are designed to function just like natural teeth, allowing for normal biting and chewing without discomfort. This level of functionality can significantly improve quality of life, especially for individuals who have struggled with ill-fitting dentures or other temporary solutions.
Aesthetic Benefits:
Endosteal implants provide the most natural-looking replacement for missing teeth. They are designed to blend seamlessly with the surrounding teeth, enhancing the smile and boosting confidence. With advancements in dental technology, the aesthetic results of implants continue to improve, offering an even more convincing natural appearance.
Versatility:
Whether replacing a single tooth, several teeth, or supporting full dentures, endosteal implants offer a versatile solution adaptable to various dental needs. Their flexibility makes them suitable for a wide range of patients, addressing specific challenges with customized implant strategies.
In summary, the advantages of endosteal implants are multifaceted, addressing not only the aesthetic concerns associated with tooth loss but also promoting better oral health, preserving jawbone integrity, and restoring full functionality. These benefits solidify endosteal implants as the standard in implant dentistry, offering a reliable, long-term solution for patients seeking to enhance their oral health and quality of life.
The Procedure of Placing Endosteal Implants
The process of placing endosteal implants is meticulous and requires a series of steps to ensure the success and longevity of the implant. It involves careful planning, surgical placement, and a period of healing before the final restoration can be attached. Here’s an overview of what patients can expect during the endosteal implant procedure:
1. Initial Consultation and Planning: The journey to getting endosteal implants begins with a comprehensive evaluation by a dental professional. This step includes dental exams, X-rays, and possibly 3D imaging to assess the health of the jawbone and to plan the implant placement. The dentist will discuss the patient’s medical history, oral health, and treatment expectations to ensure they are a suitable candidate for implants.
2. Preparatory Procedures (If Necessary): Some patients may require preparatory procedures before the implant can be placed. This could include bone grafting to enhance the jawbone where bone density is insufficient or tooth extractions if necessary.
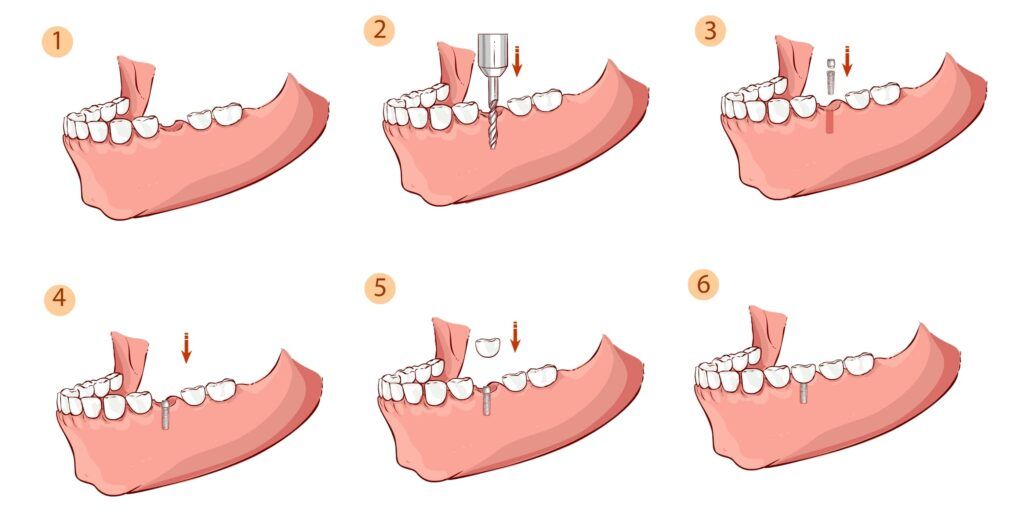
3. Surgical Placement of the Implant: The actual placement of the endosteal implant is a surgical procedure that is usually performed under local anesthesia, with sedation options available for patients who may need them. The dentist or oral surgeon makes an incision in the gum to expose the bone and then drills a hole where the implant will be inserted. The titanium or zirconia implant is placed into the jawbone, and the incision is sutured closed.
4. Healing and Osseointegration: After the implant is placed, a period of healing is required, which can last several months. During this time, the process of osseointegration occurs, where the jawbone grows around and bonds with the implant. This critical phase ensures the implant becomes a stable and permanent part of the jaw.
5. Attaching the Abutment: Once osseointegration is complete, a second minor surgery might be necessary to attach an abutment to the implant. The abutment serves as a connection point for the final crown or prosthetic tooth. In some cases, the abutment can be placed during the initial surgery.
6. Placement of the Prosthetic Tooth or Teeth: After the gum tissue has healed around the abutment, impressions of the mouth are taken to create a custom crown, bridge, or denture, which will be attached to the implant(s). This final restoration is designed to match the color, shape, and size of the surrounding teeth, ensuring a natural and aesthetically pleasing result.
7. Follow-Up and Care: After the placement of the prosthetic, follow-up visits are essential to monitor the implant, adjust the fit of the prosthetic if necessary, and to ensure the patient is maintaining good oral hygiene practices to support the longevity of the implant.
The procedure for placing endosteal implants is a testament to the advancements in dental technology and techniques, offering patients a highly effective and lasting solution for tooth loss. While the process can be lengthy, the outcome is a durable, functional, and natural-looking restoration that can significantly improve a patient’s quality of life.
Comparing Endosteal Implants with Other Restoration Types
Here’s a table that compares endosteal implants with other types of dental restoration options on several key features:
| Feature | Endosteal Implants | Subperiosteal Implants | Dentures | Dental Bridges |
| Placement | In the jawbone | On top of the jawbone under the gum | On the gum, removable | Attached to adjacent teeth |
| Bone Requirement | High (adequate bone density needed) | Lower (suitable for patients with insufficient bone height) | Not applicable | Not applicable |
| Stability and Durability | Very high | Less than endosteal implants | Varies, generally lower due to lack of bone integration | High, but depends on the health of adjacent teeth |
| Aesthetic and Functional Outcome | Most natural-looking and functional | Good but can be less natural than endosteal implants | Good, but may not match the natural appearance and function of endosteal implants | Good, but involves alteration of adjacent teeth |
| Preservation of Oral Health | Does not require alteration of adjacent teeth, prevents bone loss | Does not require alteration of adjacent teeth, but does not prevent bone loss as effectively | May cause additional bone loss over time, no impact on adjacent teeth | Requires alteration of adjacent teeth which may affect their long-term health |
| Procedure Complexity | More complex, may involve multiple steps including bone grafting | Less complex than endosteal but more so than dentures | Least complex, non-surgical | Moderately complex, involves preparation of adjacent teeth |
| Long-Term Success Rate | Very high | Lower than endosteal implants | Varies, frequent adjustments or replacements may be needed | High, but less than endosteal implants due to potential damage to supporting teeth |
This comparison highlights the distinctive advantages and considerations associated with each dental restoration
FAQ: Endosteal Implants
1. What are endosteal implants?
Endosteal implants are a type of dental implant designed to replace missing teeth. They consist of a titanium or zirconia post that is surgically placed into the jawbone, acting as an artificial root. Once the implant integrates with the bone, a process known as osseointegration, a prosthetic tooth (crown) is attached to the post, providing a stable and natural-looking replacement for the missing tooth.
2. How long does the endosteal implant process take?
The duration of the endosteal implant process can vary widely depending on individual circumstances, including the patient’s oral health, the need for any preparatory procedures such as bone grafting, and the speed of healing. Typically, the process can take anywhere from three to six months. This timeline allows for the surgical placement of the implant, the healing period for osseointegration, and the attachment of the abutment and crown.

3. Are endosteal implants painful?
Patients are usually under local anesthesia during the implant surgery, which minimizes pain during the procedure. Post-operative discomfort is normal but is generally manageable with over-the-counter pain relievers or prescribed medications. Most patients report that the discomfort is less than they anticipated and decreases significantly within a few days after the procedure.
4. How successful are endosteal implants?
Endosteal implants have a high success rate, often exceeding 95% over a 10-year period. Success rates vary depending on various factors, including the location in the jaw, the patient’s overall health, and adherence to good oral hygiene practices. Factors like smoking or untreated chronic diseases can lower the success rate.
5. How do I care for my endosteal implant?
Caring for endosteal implants involves maintaining good oral hygiene practices similar to those for natural teeth. This includes brushing twice a day, flossing daily, and using an antimicrobial mouthwash as recommended by your dentist. Regular dental check-ups and cleanings are also crucial for monitoring the health of the implant and the surrounding gum tissue. Proper care can significantly extend the life of your implant.
These FAQs cover the basics of what potential candidates need to know about endosteal implants, providing a solid foundation for making informed decisions about this effective tooth replacement option.
Conclusion
In conclusion, endosteal implants represent the pinnacle of dental implant technology, offering unmatched durability, versatility, and the ability to restore not just the appearance but the functionality of natural teeth. Their role as the standard in implant dentistry is well-earned, thanks to the comprehensive benefits they provide to patients seeking long-term solutions for tooth loss. Whether you are exploring dental implants for the first time or considering your options, endosteal implants merit serious consideration for their ability to improve oral health, enhance quality of life, and offer a permanent solution to missing teeth. We encourage you to reach out to your dental professional to discuss whether endosteal implants are the right choice for you. By scheduling a consultation, you can take the first step towards restoring your smile with the confidence and assurance that comes from choosing the gold standard in implant dentistry.

