When COVID-19 first arrived in the United States in late 2019, preventive measures such as wearing masks and staying 6 ft apart from one another were relatively unfamiliar to many people. By now, however, these practices have been commonplace in areas where the virus is actively spreading. These practices are based on the theory that COVID-19 is primarily spread through respiratory droplets in the air that are inhaled into the lungs. Although this theory remains the most prominently accepted explanation for how the SARS-CoV-2 virus spreads, researchers have developed another hypothesis for how the virus reaches the lungs. This new hypothesis also aims to address the question of why certain people develop complications associated with COVID-19 while others do not.
Instead of the SARS-CoV-2 virus being directly delivered to the lungs through inhalation, this new hypothesis proposes that the virus is transmitted from the mouth into the lungs via the bloodstream. Building on this idea, the hypothesis also notes that an individual’s oral health may be a way to predict who is at a higher risk of developing COVID-19 lung disease. This hypothesis was recently published in the Journal of Oral Medicine and Dental Research and is titled, The COVID-19 Pathway: A Proposed Oral-Vascular-Pulmonary Route of SARS-CoV-2 Infection and the Importance of Oral Healthcare Measures.
The article starts out by first addressing shortcomings in the theory that SARS-CoV-2 is delivered to the lungs through the airways and instead postulates that it is delivered to the lungs through the bloodstream. One of the main arguments the article raises in opposition to the theory that SARS-CoV-2 is delivered directly into the lungs through the airways is the fact that studies have identified the initial infection starts in the upper airway, specifically the nasal passages, and not the lungs. Another argument the article brings forth is that the distribution of lung disease associated with COVID-19 does not resemble lung disease from an inhaled pathogen. This is because COVID lung disease primarily forms in the base of the lungs, while other inhaled forms of lung disease are uniformly distributed throughout all areas of the lungs. This implies that there must be some other way in which the virus is transmitted to the lungs.
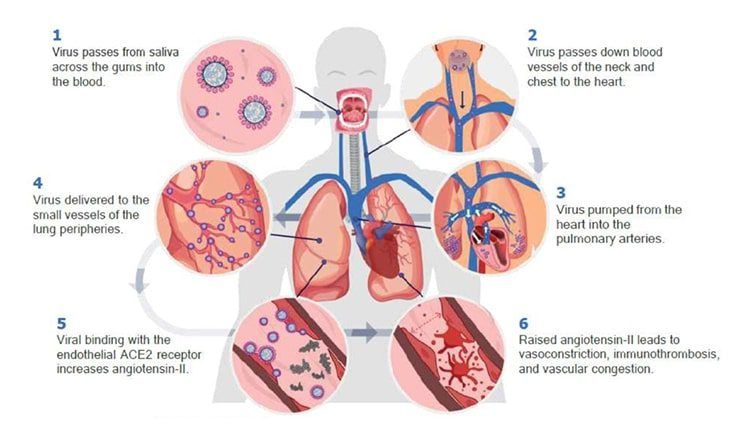
Instead, it is suggested by the article that the oral cavity serves as a reservoir of SARS-CoV-2 and that the virus is able to breach the immune defense barrier in order to enter the bloodstream. Once entering the bloodstream through the mouth, the virus travels down through the veins of the neck and chest into the heart, where it is then pumped into the pulmonary arteries and the small vessels in the lung periphery.
This new hypothesis is supported by radiological findings that have identified dilated blood vessels in the lungs in association with ground-glass opacities that were the hallmark sign of COVID-19 in the early days of the pandemic. These dilated blood vessels are believed to cause the formation of abnormal vascular structures that connect a pulmonary artery to a pulmonary vein, bypassing the pulmonary capillary bed. This is known as a pulmonary arteriovenous malformation and it is thought to be one of the reasons why people with COVID-19 have less oxygen content in their blood.
Another finding that suggests SARS-CoV-2 travels through the bloodstream is the high incidence of pulmonary thromboembolic disease in COVID-19 patients. Pulmonary thromboembolic disease is characterized by blood clots that migrate from the systemic bloodstream into the pulmonary blood vessels. In COVID-19 patients, pulmonary thromboembolic disease varies slightly from conventional pulmonary thromboembolic disease. Specifically, patients with COVID-19 who develop pulmonary thromboembolic disease have filling defects that are lower in volume and found on the edges of the lungs. This suggests the presence of immunothrombosis, which is an immune response whereby the body uses the production of a blood clot to trap pathogens in a specific area of tissue to prevent these pathogens from spreading throughout the body.
After discussing various radiological findings that suggest SARS-CoV-2 reaches the lungs through the bloodstream, the article then explains how the virus moves into the bloodstream from the oral cavity. The article notes that key elements for COVID infection are abundantly found in the gingival tissues, minor salivary glands, and tongue. This means that the virus can infect and collect within these oral structures. One study suggests that the virus can remain in saliva for over two months and that high saliva viral load can be used as a predictor of poor outcome. Since SARS-CoV-2 can accumulate in the saliva, this increases the risk of the gums becoming infected.
There are several past studies that have demonstrated the presence of human viruses in saliva, gingival crevicular fluid (GCF), subgingival plaque, and gingival tissues. These viruses include: human immunodeficiency virus, herpesvirus, Epstein-Barr virus, cytomegalovirus, and Zika virus. A recent study has also shown that SARS-CoV-2 RNA was found in the gingival crevicular fluid in 64% of COVID-19 positive patients. It is important to note that gingival crevicular fluid is produced as an anti-inflammatory response to periodontal disease and people with healthy gums generally have very little GCF.
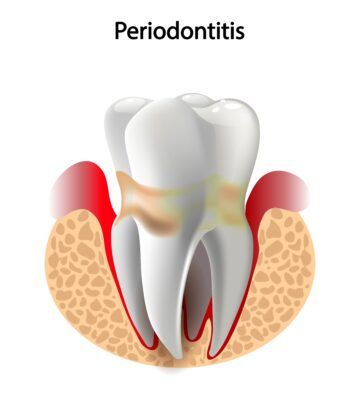
Researchers believe that viral particles are able to migrate into periodontal pockets. Periodontal pockets form when gum inflammation causes the gums to pull away from the teeth, creating a space between the tooth root and soft tissue. Periodontal pockets provide an ideal environment for the viral particles to survive, allows for viral replication, and can cause SARS-CoV-2 to spread to the gingival capillaries. It is also believed that the local inflammation caused by periodontal disease greatly increases the risk of the virus passing through the pocket epithelium to the bloodstream. Many previous studies have shown that excess bacterial loads can overwhelm the immune defenses of the mouth, allowing the bacteria to enter the bloodstream. It is now believed that viruses, such as SARS-CoV-2, can do the same.
Unfortunately, there have already been some studies that have found that periodontal disease increases the risk of COVID-19 complications. The article attributes this phenomenon to the fact that periodontitis causes both local and systemic inflammation, which triggers the release of pro-inflammatory cytokines. Studies have shown that systemic inflammation directly affects the severity of COVID-19, with the risk for respiratory failure being 22 times greater in patients with higher levels of the inflammatory cytokine IL-6.
Furthermore, the article also points out the close link between periodontitis and other respiratory conditions such as pneumonia and chronic obstructive pulmonary disease (COPD). For starters, otherwise healthy individuals with periodontitis show decreased lung volume, airflow limitation, and worse pulmonary function. Additionally, it has also been shown that periodontitis increases the risk of developing respiratory conditions such as pneumonia and COPD. This relationship between periodontitis and respiratory conditions implies that treating periodontitis can decrease the severity of pulmonary infection. This is built upon the notion that periodontal treatment has helped improve systemic inflammation in people with chronic diseases such as type-2 diabetes, hypertension, coronary heart disease, and atherosclerosis. The article also notes that dental plaque could be a constant source of viral delivery to the lungs, which could result in poorer outcomes.

Although the information presented in this article is still hypothetical, it could change our understanding of the SARS-CoV-2 virus, specifically in terms of how we could prevent or decrease the severity of COVID-19 infections. This article suggests that decreasing the viral load in saliva could help to decrease the risk of severe infections resulting in lung infections and death. The viral load found in saliva can be decreased by optimal oral hygiene practices: brushing twice a day with fluoridated toothpaste, using interdental brushes between the teeth, and visiting the dentist to manage cases of periodontal disease. Certain mouthwashes have also been suggested as a way to kill the SARS-CoV-2 virus in the saliva and decrease the risk of it entering the bloodstream.
The article concludes by promoting the use of oral hygiene practices as a way of preventing or reducing the severity of COVID-19 lung infections. From a dental standpoint, improving your dental hygiene practices can only improve your oral health, and in this case, possibly your ability to combat the SARS-CoV-2 virus. So, mask up, stay six feet apart, and don’t forget to brush and floss.

