Gum health is not merely a component of oral well-being; it is the cornerstone of successful dental implantation. Just as a sturdy house requires a solid foundation, dental implants demand healthy gums for both initial integration and long-term stability. The hidden link between the integrity of the gums and the triumph of dental implants is profound, reflecting a symbiotic relationship where one invariably influences the other. This relationship underscores the importance of periodontal health, not only for natural teeth but also as a critical determinant of whether the advanced solution of dental implants becomes a durable reality or a compromised endeavor. In exploring this connection, we delve into the multifaceted role that gum health plays—from ensuring the proper fusion of the implant to the bone, to preventing postoperative complications, and maintaining the overall aesthetic and functional outcome of dental restoration procedures.
Foundations Matter: The Role of Gum Health
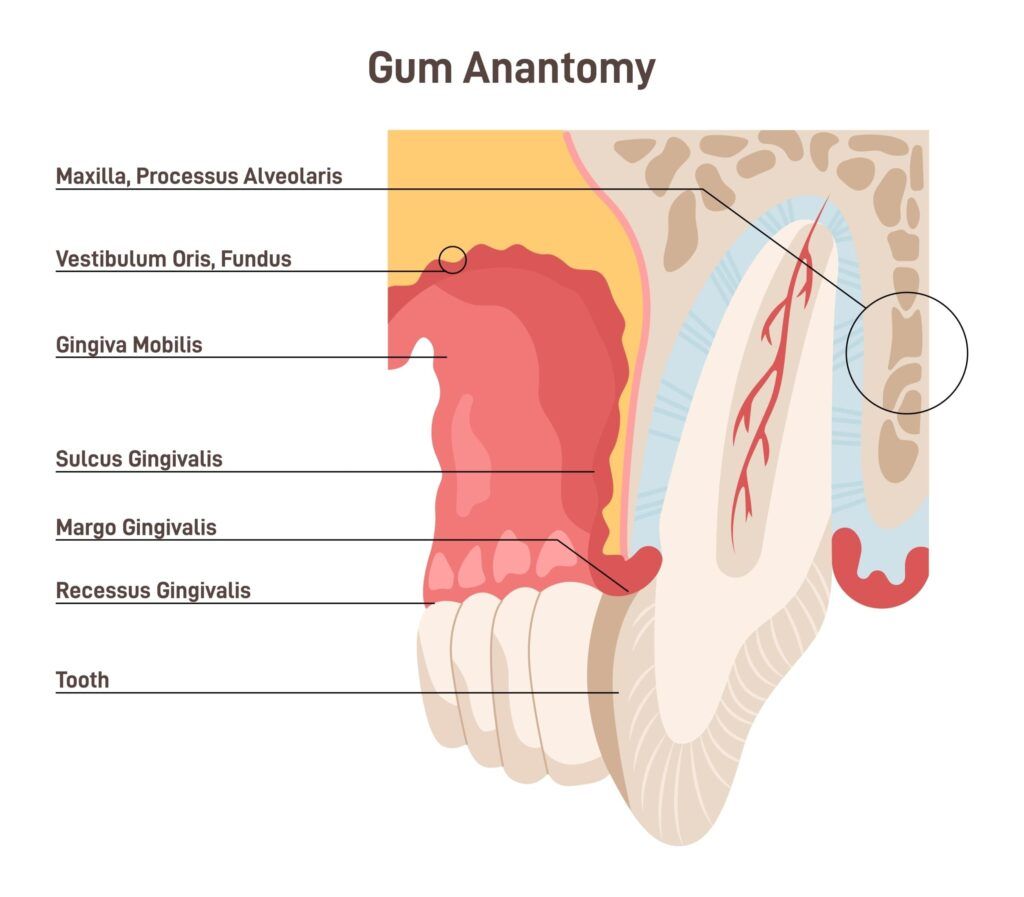
Gum health is the bedrock upon which dental implants must be secured. The gums, or gingiva, along with the underlying bone structure, are analogous to the soil and bedrock that must firmly anchor the roots of a tree. When gums are inflamed or diseased, it’s like soil that’s eroded or unfit for growth.
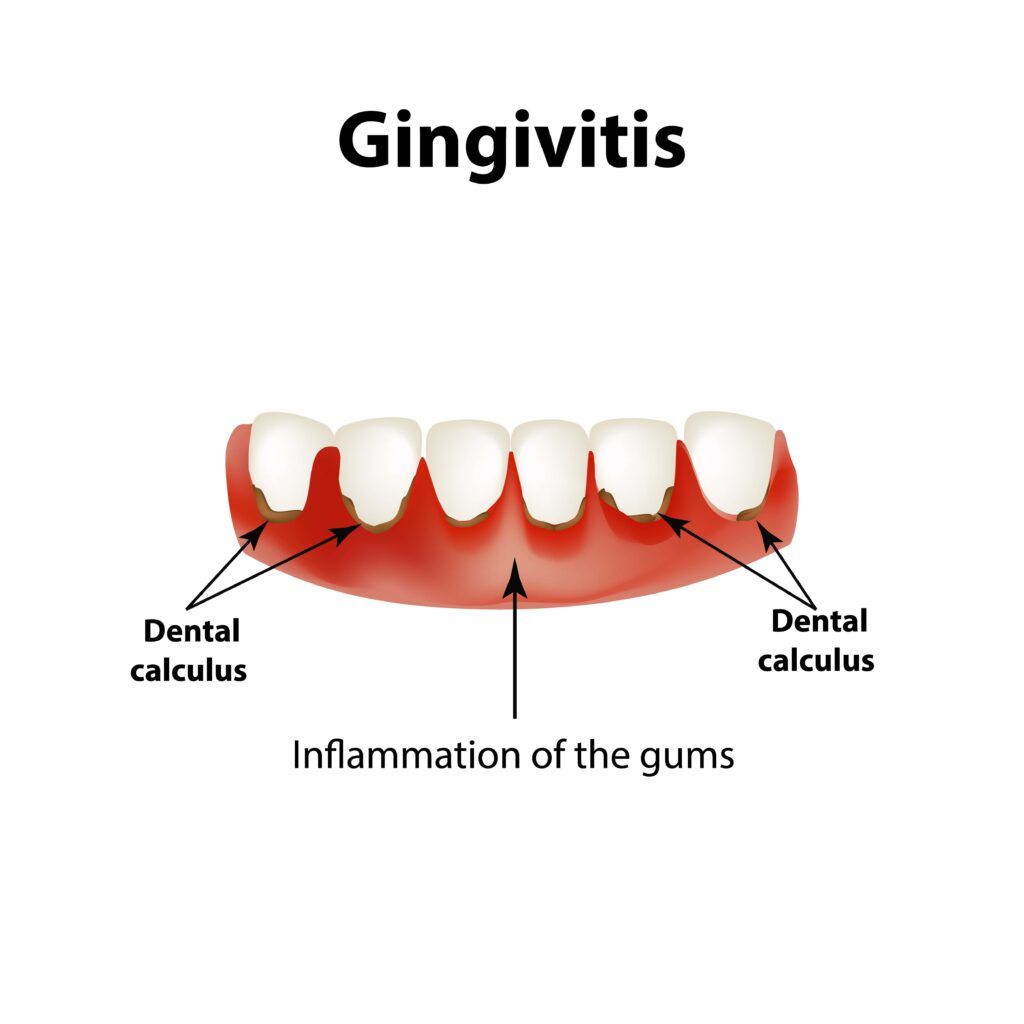
Periodontal disease is a common enemy of dental implant success. It silently erodes gums and bone, often without pain, leading to a weakening of the necessary support for an implant. To understand the correlation, let’s delve into the specifics of gum health and how it influences the lifespan of a dental implant.
Unpacking the Link: Gum Health and Implant Integration
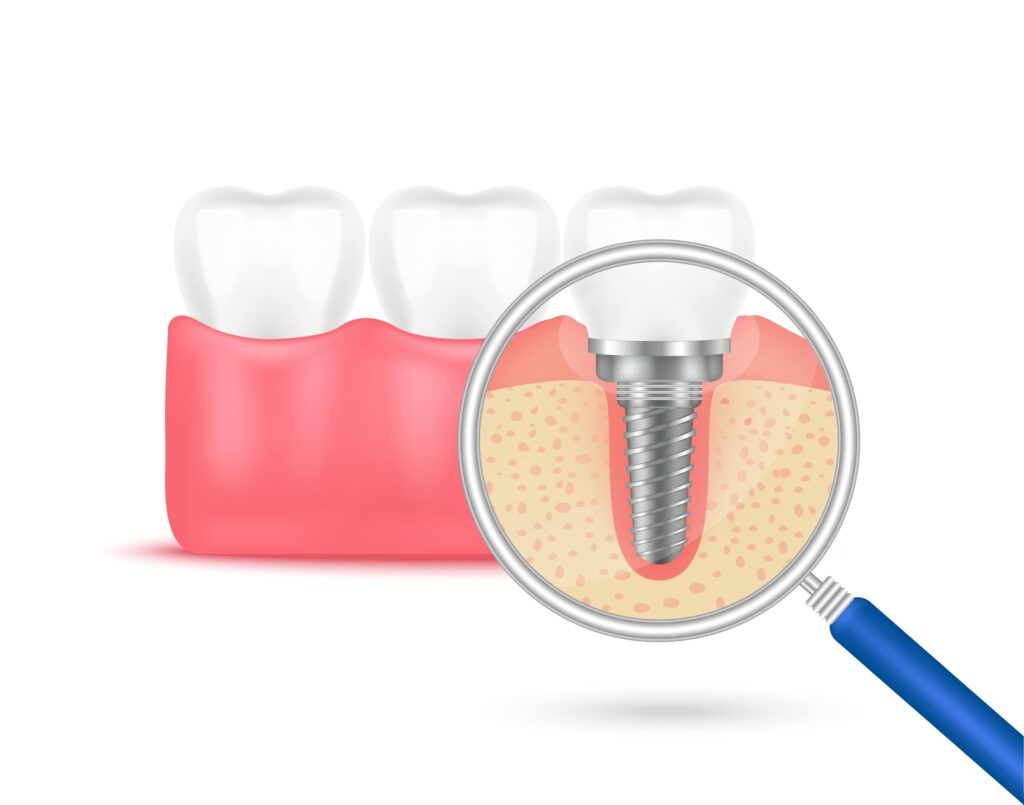
The link between gum health and the successful integration of a dental implant is a vital one, rooted in the body’s response to oral surgery and the healing process that follows. When a dental implant is placed into the jawbone, it begins a period of healing known as osseointegration, during which the bone tissue fuses with the titanium implant surface to create a sturdy base for the prosthetic tooth that will sit atop it.
Healthy gums are crucial to this process for several reasons:
Barrier Against Infection:
Healthy gums provide a protective barrier against bacteria, reducing the risk of post-surgical infection. When the gums are infected or inflamed (as in the case of periodontitis), this barrier is compromised, and bacteria can more easily penetrate the surgical site, potentially leading to implant failure.
Support for the Implant:
The gums help to hold the dental implant in place during the initial stages of healing. If the gum tissue is unhealthy, it may not be able to perform this role effectively, which can cause instability in the implant and hinder the osseointegration process.
Blood Supply:
Healthy gums have a rich blood supply, which is essential for healing after implant placement. The blood delivers nutrients and oxygen to the surgical site, which facilitates bone growth and integration. Conversely, diseased gums can have impaired circulation, leading to poor healing and less successful implant integration.
Indicator of Bone Quality:
Often, poor gum health is a sign of poor bone quality, as the same bacterial infections that destroy gum tissue can also lead to bone loss. Since dental implants need sufficient bone to anchor into, compromised bone can fail to provide the required support for an implant.
Foundation for Long-Term Success:
Long-term success of implants is not only about the initial osseointegration but also about maintaining bone and gum health around the implant. Peri-implantitis, a condition akin to periodontal disease that affects the tissue surrounding an implant, can develop if the gums are not kept healthy, leading to the deterioration of supporting bone over time.
Because of this intimate connection, dentists often require that any active gum disease be fully treated and under control before proceeding with an implant placement. Additionally, they may suggest improving and maintaining rigorous oral hygiene practices to ensure the gums are in optimal condition to support the implant for years to come. Thus, the success of a dental implant is not a singular event at the time of surgery but a continuous process that relies heavily on the health of the surrounding gum tissue.
Maintaining the Balance: Prevention and Care
The old adage “prevention is better than cure” holds especially true here. The following are pivotal steps in maintaining gum health for implant success:
- Regular Dental Check-Ups: Regular visits to the dentist can catch early signs of gum disease before they escalate to a level that can compromise implant success.
- Optimal Oral Hygiene: A regimented oral hygiene routine that includes brushing twice daily, flossing, and using an antibacterial mouthwash can significantly mitigate the risk of periodontal disease.
- Quit Smoking: Smoking is notorious for contributing to poor gum health and can negatively impact the healing process post-implant surgery.
- Managing Health Conditions: Chronic conditions such as diabetes, when uncontrolled, can affect gum health. Managing such conditions is key to maintaining a healthy environment for an implant.
The Warning Signs: Recognizing Gum Trouble
Identifying potential issues early can make all the difference. Look out for signs of gum distress, such as:
- Red, swollen, or tender gums
- Gums that bleed during brushing or flossing
- Persistent bad breath or a bad taste in the mouth
- Receding gums
- Loose teeth or a change in the way teeth fit together when biting
Getting Dental Implants with Gum Disease
While gum health is important for the success of dental implants, having gum disease does not automatically mean dental implants are impossible. However, there are some specific steps and considerations that one should take:
Consultation with a Dental Professional:
Begin with a comprehensive dental evaluation. A dentist or periodontist (a dentist who specializes in treating gum disease) will assess the extent of the periodontal disease and discuss your oral health history and options for treatment.
Treating Periodontal Disease:
Before considering implants, the active gum disease must be managed and brought under control. Treatment can include:
- Deep cleaning procedures such as scaling and root planing to remove tartar and bacteria from below the gum line.
- Medications to control infection and pain, or to aid in healing.
- Surgery to regenerate lost bone and tissue in severe cases of periodontitis.
Reevaluation of Gum Health:
After periodontal treatment, the dentist will reevaluate your gum health to determine if the disease has been successfully treated and whether the gums have healed sufficiently to proceed with implants. This may include measuring the depth of gum pockets, checking for bleeding, and assessing bone density.
Developing a Comprehensive Dental Plan:
Once your periodontal health is deemed adequate, your dental care provider will develop a detailed plan for your dental implants. This plan will include a timeline, cost estimate, expected outcomes, and any preparatory procedures needed to optimize the jawbone for implant placement, such as bone grafting.

Implementing Pre-Implant Preparations:
If there’s insufficient bone to support the implant, due to the periodontal disease, a bone graft or sinus lift may be necessary. These procedures can help build up the bone to create a solid foundation for the implants.
Placement of Dental Implants:
When your gums are healthy and there’s enough bone to secure the implants, your dentist or oral surgeon can proceed with the implant surgery. The post-implant care plan will emphasize maintaining impeccable oral hygiene and regular dental check-ups.
Ongoing Maintenance and Care:
After the implants are placed, diligent oral care is crucial. This includes:
- Regular brushing and flossing to keep the gum tissue clean.
- Periodic follow-ups with your dental dentist to monitor the health of the implants and the surrounding tissue.
- Professional cleanings and examinations at intervals recommended by your dentist.
Lifestyle Adjustments:
It’s essential to make lifestyle changes that support oral health, like quitting smoking, controlling diabetes, or other conditions that may affect gum health, and avoiding practices that put stress on the dental implants.
Monitoring for Peri-Implantitis:
Be vigilant for signs of peri-implantitis, which is similar to periodontal disease but affects the tissues surrounding an implant. Prompt treatment can help save the implant and prevent further complications.
It’s critical to understand that while treating periodontal disease is the first step towards dental implants, maintaining gum health is an ongoing commitment. Successful dental implants require a lifelong dedication to oral hygiene and professional care. With careful planning and treatment, even those who have suffered from periodontal disease can enjoy the benefits of dental implants.
Conclusion
In conclusion, while dental implants offer a viable solution for tooth loss, their longevity is intricately tied to the health of the gums. By maintaining gum health, we not only ensure the success of dental implants but also uphold the integrity of our overall oral well-being. As research progresses and methods improve, we stand on the cusp of a future where implant failure due to poor gum health could become a rarity rather than a risk—a future where the smile you gain today will be the one you wear for years to come.