Many people assume that getting dental implants eliminates the need for proper oral hygiene, especially since they cannot be damaged by tooth decay like natural teeth. Although it is true that dental implants and the attached prosthesis do not decay, problems can still arise when plaque accumulates on or around the implant or prosthesis. Since this is the case, it is important to know the basic facts on plaque, as well as how plaque can affect your dental implants.
What is plaque?
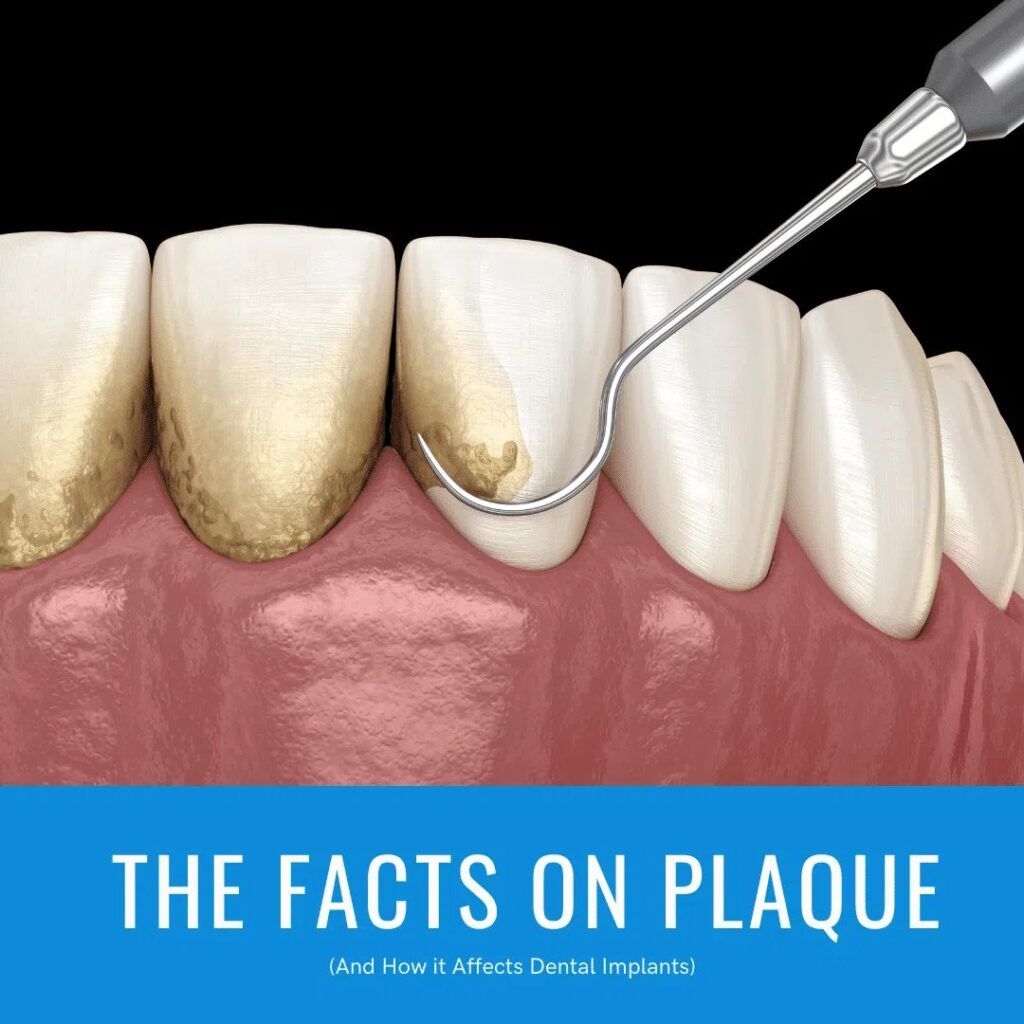
Before getting into how plaque affects your implants, it is important to first understand the basics on what makes up plaque. If you’ve ever noticed soft buildup on the surface of your teeth or felt the sensation of having “fuzzy” teeth, then you have experienced plaque. Dental plaque is the clear, sticky film that forms all over the surface of your teeth (or dental restoration). Although it is normally clear, plaque can become slightly colored when it collects food debris.
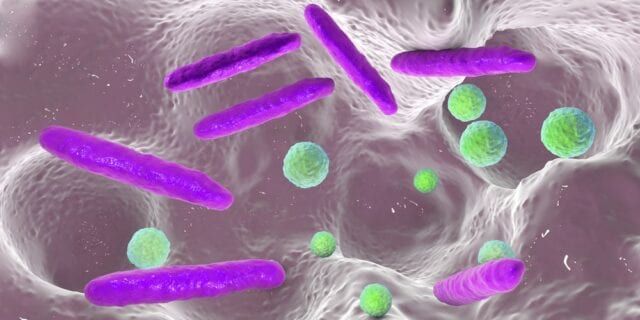
Plaque is primarily composed of water, however if you were to dry plaque, the remaining components are 70% bacteria and only 30% polysaccharides and glycoproteins. Because of this, plaque is sometimes referred to as microbial plaque, oral biofilm, dental biofilm, dental plaque biofilm, or bacterial plaque biofilm. In fact, researchers have discovered around 1,000 different types of bacteria that regularly reside within dental plaque.
Where does plaque form?
Plaque can form anywhere on the tooth or dental restoration surface. There are actually two types of plaque that are differentiated based on where they form. The first type of plaque is known as supragingival plaque, which forms above the gum line. Supragingival plaque often forms in between the teeth, within the pits and fissures of molars, and along the gum line. It is also the first type of plaque to form about 4-12 hours after brushing or flossing.
When supragingival plaque is not removed with proper brushing or flossing, then it can spread into subgingival plaque. Subgingival plaque forms under the gum line when bacteria from supragingival plaque migrate down below the gum line. When it comes to the health of your dental implants, subgingival plaque can cause some serious complications.
What causes plaque to form?
The formation of dental plaque is natural, especially considering that its two main components, water and bacteria, are always present in the mouth. Additional bacteria can also be added to the mouth while eating, drinking, and breathing, which can lead to the development of more plaque. New plaque is able to develop because your mouth provides an ideal environment for bacteria to thrive and reproduce.

One reason is because the pH of your saliva is around 6 and 7, while the ideal pH for plaque growth is between 6.7-8.3. Another reason is because teeth (and dental restorations) do not shed like other parts of the body, meaning that plaque can continue to accumulate without being disturbed. The only way to disturb and remove plaque is with regular brushing and flossing. Without proper brushing and flossing, however, plaque will continue to grow and spread over the surface of your teeth, restoration, and the implant.
Although plaque is soft and can easily be removed with a toothbrush, it can harden if left undisturbed for too long. This is because your saliva contains various minerals that are deposited on plaque. Unfortunately, these minerals end up hardening dental plaque, turning it into dental calculus, or tartar. While plaque normally forms about 4-12 hours after brushing, tartar normally forms about 24-72 hours after plaque forms. Since tartar essentially hardens and bonds plaque to your enamel, it cannot be removed with simply brushing and flossing, and can only be removed by your dentist with special tools.
How Plaque Affects Your Dental Implants
When it comes to dental plaque, two of the biggest threats to your oral health are tooth decay and gum disease. This is because as plaque accumulates on the surface of natural teeth, it produces an acidic waste product that gradually wears down the enamel and allows bacteria to enter the tooth. Unlike natural teeth, however, the dental prosthesis used with dental implants are not susceptible to decay and will not wear down over time in response to plaque.
However, dental implants can still be adversely affected by plaque in the form of gum disease. Gum disease occurs when too much bacteria from plaque causes inflammation and infection of the gum tissue. When only the gums are affected, this is known as gingivitis and it can usually be reversed with proper treatment. In cases where gingivitis is not treated, however, the infection can spread to the other supporting structures such as the cementum, alveolar bone, and periodontal ligaments. At this point, the infection is known as periodontitis.
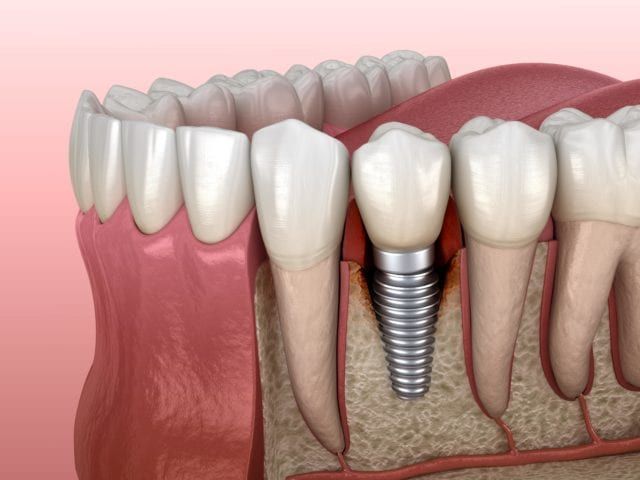
After having dental implants placed, you will no longer need to be concerned about cementum or periodontal ligaments, since these are both removed with your natural teeth before the implant is placed. However, this does not mean that you are immune to gum disease. When excess plaque forms along the gum line (or spreads below the gum line), it will cause the gum tissue to become infected and can lead to gum recession. When the gums start to pull away from the prosthetic, they form pockets for more plaque and bacteria to accumulate. They also allow bacteria to surround the implant, which can lead to peri-implant mucositis or peri-implantitis.
Peri-implant mucositis and peri-implantitis are two types of peri-implant diseases that can affect the soft and hard tissues around the implant. Peri-implant mucositis is characterized by gum inflammation with no bone loss. When caught early, peri-implant mucositis can be treated and usually reversed. Peri-implantitis, on the other hand, is characterized by soft tissue inflammation and bone deterioration. This can occur because chronic inflammation from the infection causes an auto-immune response whereby the body starts attacking the alveolar bone. Since the implants are fused into the alveolar bone, they can become loose if this bone starts to deteriorate. This can eventually lead to implant failure.
How to Manage Plaque
Your implant dentist will provide you with detailed information on how to care for your dental implants by managing plaque. Generally speaking, you can manage plaque by brushing your “teeth” twice a day and flossing daily. However, flossing with dental implants may vary slightly from traditional flossing. For example, your implant dentist may recommend avoiding traditional dental floss and instead using an interdental brush or water flosser. Additionally, it is also important to schedule regular dental exams with dental implants so your implant dentist can help you manage your oral health and ensure your implants are staying healthy. Your implant dentist can also clean around the implant and the dental prosthetic (crown, bridge, or denture) to remove excess plaque and tartar buildup in order to decrease the risk of peri-implant diseases and implant failure.